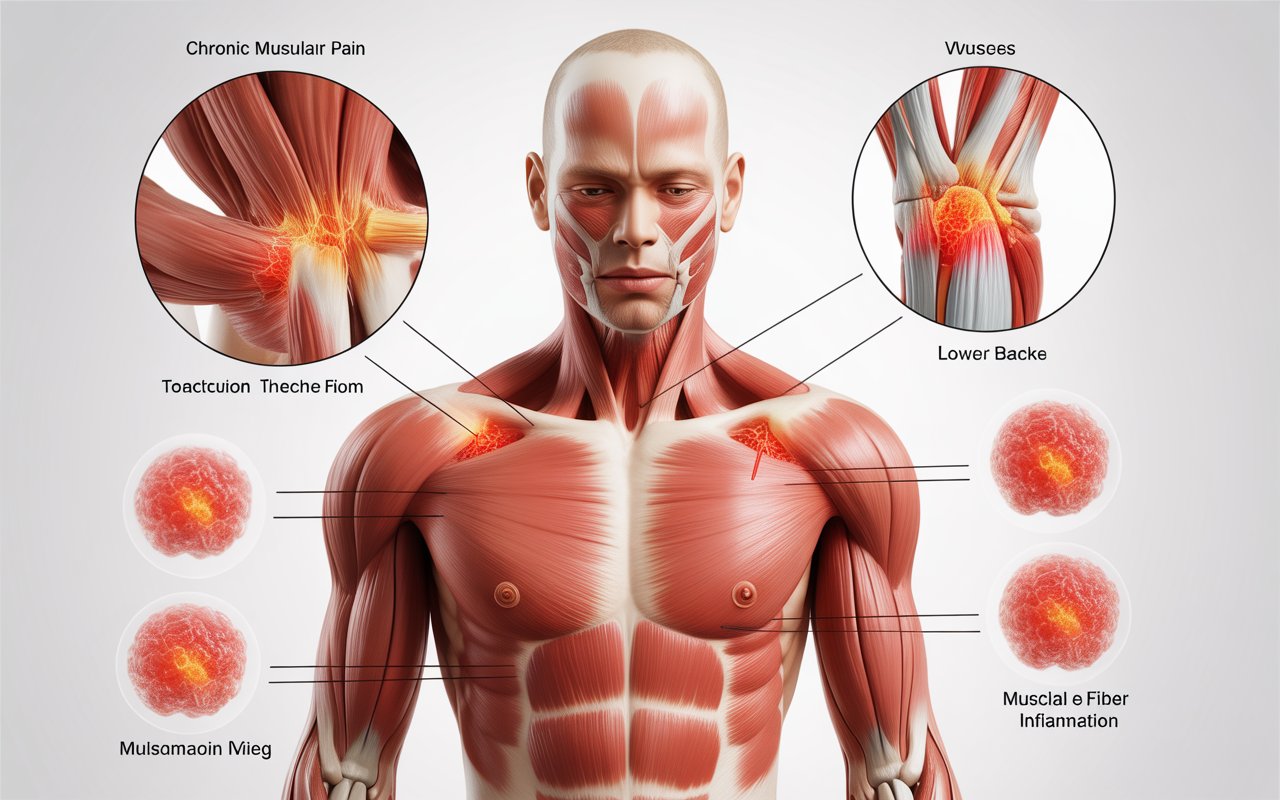
Chronic Muscle Pain and Inomyalgia: What You Need to Know
Chronic muscle pain disorders affect millions of people worldwide, often diminishing quality of life and causing physical and emotional strain. While conditions like fibromyalgia are widely recognized, there exists a lesser-known condition called Inomyalgia, which shares some similarities with other chronic pain disorders but has its own unique characteristics.
Understanding it is essential for patients experiencing its symptoms, caregivers supporting them, and healthcare providers aiming for an accurate diagnosis and effective management. This guide explores the causes, symptoms, diagnosis, treatment options, and coping strategies for it, providing a thorough overview to empower individuals navigating this challenging condition.
What Is Inomyalgia?
It is a chronic disorder characterized by persistent muscle pain, fatigue, and tenderness. Unlike typical post-exercise soreness or temporary muscle aches, it involves ongoing discomfort that can affect daily activities, mental clarity, and overall well-being.
Etymology and Medical Background
The term itself provides insight into the condition’s nature:
- “Ino” – muscle or fiber
- “Myalgia” – pain
Put together, Inomyalgia translates to muscle fiber pain, emphasizing the deep, persistent nature of discomfort within muscles. While it is an emerging term in medical discussions and not yet formalized as a clinical diagnosis, it serves as a useful label for understanding a specific set of chronic pain symptoms.
How It Differs from General Muscle Soreness or Fatigue
Unlike normal muscle soreness, which typically resolves within a few days after physical activity, it pain is persistent, often occurring without a clear trigger. Fatigue associated with it is also resistant to rest, leaving individuals feeling exhausted even after sleep or relaxation.
Who It Affects
It appears to affect more women than men and typically emerges in early to middle adulthood. Factors such as high stress levels, hormonal fluctuations, poor sleep, and physical or emotional trauma are frequently associated with its onset. While anyone can develop it, understanding the demographics helps guide awareness and treatment strategies.
Importance of Distinguishing from Similar Conditions
It is often confused with fibromyalgia or other chronic pain syndromes. Accurate recognition is critical because treatment strategies may differ depending on whether the pain is localized or systemic. Misdiagnosis can lead to prolonged suffering and ineffective therapies, making awareness among patients and healthcare professionals essential.
Symptoms of Inomyalgia
The symptoms of it are multifaceted, affecting both the body and mind. They can vary from person to person and often fluctuate, making diagnosis challenging.
Physical Symptoms
- Widespread muscle pain and tenderness: Pain may start in localized muscle groups and gradually spread.
- Chronic fatigue: Persistent exhaustion not alleviated by rest.
- Morning stiffness: Difficulty moving upon waking or after inactivity.
- Sensitivity: Heightened sensitivity to touch or temperature changes.
- Headaches and muscle heaviness: A feeling of tension and weight in muscles, sometimes accompanied by mild headaches.
Cognitive and Emotional Symptoms of Inomyalgia
- Brain fog: Difficulty concentrating, forgetfulness, and slowed thinking.
- Sleep disturbances: Problems falling asleep, staying asleep, or achieving restful sleep.
- Anxiety, stress, and emotional strain: Chronic pain can contribute to mood disorders and feelings of frustration or isolation.
Symptom Variability
- Fluctuations: Individuals may experience flare-ups, periods of intensified pain, followed by periods of remission, during which symptoms are less pronounced.
- Triggers: Common triggers include physical overexertion, stress, weather changes, or hormonal shifts, making daily planning challenging.
Causes and Risk Factors of Inomyalgia
The exact cause of Inomyalgia remains uncertain, but research points to a combination of biological, environmental, and lifestyle factors.
Biological Factors
- Central sensitization: Heightened nervous system activity amplifies pain signals.
- Neurotransmitter imbalances: Altered serotonin or dopamine levels may affect both pain perception and mood.
- Genetic predisposition: Chronic pain syndromes can run in families, suggesting a hereditary component.
Environmental and Lifestyle Factors
- Chronic stress: Prolonged emotional or psychological stress increases muscle tension and pain sensitivity.
- Physical trauma or injury: Past injuries or repetitive strain may trigger persistent pain.
- Poor sleep quality: Sleep deprivation impairs muscle recovery and exacerbates fatigue.
- Sedentary lifestyle: Lack of movement can worsen stiffness and muscular weakness.
Hormonal Factors
- Menopause or post-pregnancy changes: Hormonal fluctuations may influence pain perception.
- Cortisol variations: Stress-related hormone imbalances can heighten sensitivity to discomfort.
Multifactorial Nature
It likely arises from the interaction of genetics, environment, lifestyle, and psychological factors, emphasizing the need for a holistic approach to treatment and management.
Explain the Diagnosis
Diagnosing Inomyalgia can be challenging due to the absence of specific biomarkers or definitive tests. Healthcare providers rely on a combination of clinical evaluation and exclusion of other conditions.
Diagnostic Process
- Detailed patient history: Review of symptom onset, intensity, duration, and triggers.
- Physical examination: Assessment of muscle tenderness, stiffness, and pain points.
- Exclusion of other conditions: Ruling out arthritis, thyroid disorders, fibromyalgia, and other musculoskeletal or systemic diseases.
- Imaging and laboratory tests: MRI, X-rays, and blood work help exclude structural or inflammatory causes of pain.
Importance of Knowledgeable Providers
Due to the subjective nature of pain, patients may feel dismissed or misunderstood. Consulting healthcare professionals familiar with chronic pain syndromes ensures accurate diagnosis and tailored treatment plans.
Differences Between Inomyalgia and Fibromyalgia
| Feature | Inomyalgia | Fibromyalgia |
| Pain Distribution | Often localized; may become widespread | Widespread pain in all four body quadrants |
| Core Symptoms | Muscle fiber pain, fatigue | Widespread pain, fatigue, cognitive dysfunction |
| Associated Conditions | Fewer systemic issues | IBS, headaches, multiple sensitivities |
| Diagnostic Status | Emerging term, not formal diagnosis | Established clinical diagnosis |
Common Misdiagnosis Issues
Due to overlapping symptoms like fatigue, sleep problems, and cognitive impairment, it is often mistaken for fibromyalgia or other chronic pain disorders.
Why Awareness Matters
Recognizing the unique characteristics of Inomyalgia ensures patients receive appropriate treatment strategies, avoids unnecessary therapies, and encourages research into targeted interventions.
Explain the Treatment Options
Managing it requires a multifaceted approach, combining medical interventions, physical rehabilitation, lifestyle adjustments, and alternative therapies. Since there is no permanent cure, treatment primarily focuses on reducing symptoms, improving function, and enhancing quality of life.
Medical Treatments
Medical management aims to relieve pain, improve sleep, and address associated symptoms:
- Pain relievers: Over-the-counter (OTC) medications like acetaminophen or NSAIDs may help reduce discomfort. For more severe symptoms, prescription-strength options are sometimes required under medical supervision.
- Low-dose antidepressants: Certain antidepressants help regulate neurotransmitters, improving both mood and sleep, while also reducing chronic pain perception.
- Anti-seizure medications: Drugs typically used for neuropathic pain may help calm overactive nerves and reduce muscle discomfort.
Physical Therapy and Rehabilitation
Physical therapy is a cornerstone in managing Inomyalgia, focusing on restoring movement, flexibility, and strength:
- Stretching and strengthening exercises: Targeted routines help improve muscle tone, reduce stiffness, and prevent deconditioning.
- Low-impact activities: Walking, swimming, and yoga maintain mobility while minimizing strain on muscles.
- Massage, hydrotherapy, and other techniques: Therapeutic massage and water-based exercises alleviate tension, improve circulation, and promote relaxation.
Lifestyle Adjustments
Daily habits significantly influence the severity of symptoms and overall well-being:
- Regular gentle exercise: Consistency is key. Short, frequent activity sessions help prevent stiffness and fatigue without overexertion.
- Consistent sleep routines: Prioritizing sleep hygiene—consistent bedtimes, dark and quiet environment—supports muscle recovery.
- Stress management: Meditation, deep breathing exercises, and mindfulness practices can reduce pain flare-ups triggered by stress.
- Anti-inflammatory diet and hydration: Diets rich in fruits, vegetables, lean proteins, and healthy fats can help reduce systemic inflammation. Staying hydrated supports proper muscle function.
Alternative Therapies of Inomyalgia
Many individuals benefit from complementary approaches alongside conventional treatments:
- Acupuncture: Stimulates specific points to relieve muscle pain and promote energy balance.
- Herbal supplements: Turmeric, ginger, and magnesium may help reduce inflammation and support nerve and muscle health. Always consult a healthcare provider before starting supplements.
- Mind-body practices: Yoga, tai chi, and other mindful movement techniques enhance physical flexibility, reduce stress, and improve emotional well-being.
Coping Strategies and Daily Management
Living with Inomyalgia requires practical strategies to maintain independence and manage symptoms effectively.
- Building a support system: Family, friends, and support groups provide emotional reassurance and practical help. Sharing experiences reduces feelings of isolation.
- Pacing activities and energy conservation: Breaking tasks into smaller steps, resting between activities, and avoiding overexertion prevent symptom flare-ups.
- Symptom diary: Tracking pain, fatigue, triggers, diet, and activity levels helps identify patterns and informs treatment adjustments.
- Mental health management: Cognitive-behavioral therapy (CBT), mindfulness, and counseling can improve coping skills and emotional resilience.
- Work and daily life adjustments: Ergonomic modifications, flexible work hours, and task prioritization help maintain productivity while accommodating fluctuating symptoms.
Preventive Measures
Although it cannot always be fully prevented, adopting healthy routines may reduce the risk of symptom severity:
- Maintaining good posture: Proper alignment during sitting, standing, and lifting prevents unnecessary muscle strain.
- Regular low-impact exercise: Activities like swimming, walking, or gentle yoga enhance muscle flexibility and circulation.
- Stress management techniques: Meditation, deep breathing, and mindfulness reduce muscle tension and lower the likelihood of flare-ups.
- Adequate sleep and nutrition: Consistent sleep patterns and a nutrient-rich diet support overall health and resilience.
- Regular health checkups: Monitoring hormonal and nutritional levels can prevent deficiencies that contribute to muscle pain and fatigue.
Mental Health Considerations in Inomyalgia
The connection between chronic pain and mental health is significant, as persistent discomfort can lead to anxiety, depression, and emotional strain:
- Emotional coping strategies: Mindfulness meditation, relaxation techniques, and therapy provide tools to manage stress and reduce psychological burden.
- Role of therapy: CBT and other counseling methods help reframe negative thought patterns associated with chronic illness.
- Social support: Maintaining relationships and engaging with support networks reduce feelings of isolation and provide encouragement during challenging periods.
Future Research
Ongoing research is crucial to improving understanding and treatment of Inomyalgia:
- Biological pathways and central sensitization: Studies aim to uncover how the nervous system amplifies pain signals, leading to targeted therapies.
- Genetic studies: Identifying predispositions could help in early detection and personalized interventions.
- Development of targeted therapies: Novel medications and neuromodulation techniques are being explored to specifically address related pain.
- Preventive strategies: Improved understanding of risk factors may lead to better lifestyle guidelines and interventions to minimize symptom onset or severity.
Conclusion
Inomyalgia is a complex, often under-recognized condition characterized by chronic muscle pain, fatigue, and cognitive difficulties. By understanding its symptoms, causes, diagnosis, and treatment options, patients and caregivers can take proactive steps to manage the condition effectively.
Treatment strategies include medical interventions, physical therapy, lifestyle adjustments, and alternative therapies, while coping mechanisms such as pacing, symptom tracking, and mental health support enhance daily living. Preventive measures like proper posture, exercise, stress management, and nutrition can help mitigate severity.
Awareness and accurate diagnosis are critical, as they ensure patients receive appropriate care and avoid unnecessary frustration. While no permanent cure exists yet, ongoing research offers hope for targeted therapies, preventive strategies, and improved outcomes.